Categories
Categories
Brands
Brands
- Home
- Dental Case Studies
- Steven J. Cohen DDS
Steven J. Cohen DDS
Rips, Strips and Broken Tips: Part III: Treating the Untreatable – A Case Report
 The objective of dentistry is to retain the natural dentition as part of maintaining optimum oral health. With recent studies linking oral health to general systemic health, promoting oral health translates to improved quality of life. The discipline of Endodontics encompasses retaining the dentition in the face of diseased pulp and periapical tissues.
The objective of dentistry is to retain the natural dentition as part of maintaining optimum oral health. With recent studies linking oral health to general systemic health, promoting oral health translates to improved quality of life. The discipline of Endodontics encompasses retaining the dentition in the face of diseased pulp and periapical tissues.
As endodontics is being carried out routinely in dental practice, patients are retaining their natural teeth longer. Proportionately, with an increase in successful procedures, there is also an increase in procedural complications. In Part I (May 2005) a5) and Part II (May 2006) of this article series, procedural mishaps of separated instruments and perforations were discussed in terms of management and successful treatment outcomes.
But what about years after treatment, when the only complication is that the dentistry has “worn out” so to speak? Fractured cusps, leaking margins under a 20 year old crown, and periodontal disease are possible pathways of bacterial ingress. Years after treatment where bacterial contamination has recurred, different treatment modalities have been developed to address the once treated canal system – retreatment, apical surgery and re-surgery, and extraction/implant. Part III of this series is a case report involving recurring infection years after orthograde (conventional) and retrograde (apical surgery) canal treatment of two central incisors.
CASE REPORT
A 51-year-old male presented to private endodontic practice for a second opinion regarding teeth 1.1 and 2.1. His medical history was significant for asthma and sinus problems, but no current activity.
CLINICAL FINDINGS
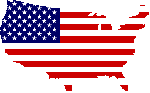
Examination revealed full crown 1.3 to 2.3 inclusive, large metal posts or silver points in 1.1 and 2.1, root lengths shortened by apical surgery, and radiolucent lesions at both 1.1 and 2.1 apices. Soft tissue displayed apical gingival scar from incision for apical surgery buccal to the central incisors, blue “tattoo” from metal corrosion, staining the gingiva apical to these two teeth, and a fistula mid-buccal at tooth 1.1.
TREATMENT OPTIONS AND CONSENT
After a 43-year history and three endodontic procedures, extraction and replacement via implant was recommended as the easiest and most definitive treatment option to resolve this problem. However, the patient wanted to explore all possibilities.
Communication with the referring dentist revealed that after the last apical surgery, healing was presumed from lack of symptoms or fistula, and the new crowns were placed for improved cosmetics and fit. Since these crowns are new, replacement was to be avoided if possible. Apical surgery had reduced the root length, and resulted in metal objects now in contact with periapical tissue and fluid, with no sign of a retroseal. A 2nd apical surgery would result in resection of the root across the metal canal filling (post or silver point), and an impossible retroseal situation. Further, the suspicion of canal contamination from the original crowns needed to be addressed.
The option of access through these crowns was discussed, with the goal to retrieve the metal pieces, medicate the canals with calcium hydroxide, and allow time for decontamination (resolution of the fistula). Once that is achieved, the canals could be obturated again. If symptoms or the fistula failed to resolve, treatment would be aborted, and extraction would be recommended. After some lengthy discussion, the patient wanted to try and salvage these two teeth, and consented to another endodontic approach.
Appointment 1
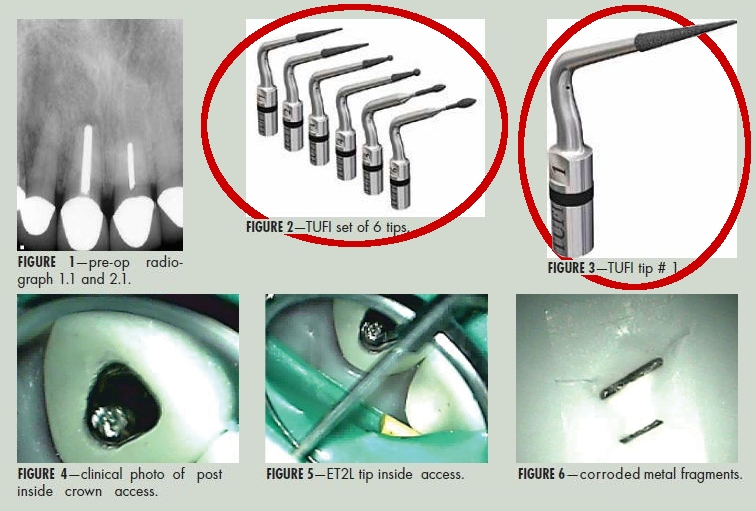
Access was made lingual through the crowns on 1.1 and 2.1, with a Tri-Hawk Talon 12 bur. The composite cores were immediately encountered under the crown surface. The composite was carefully removed incrementally using TUFI Ultrasonic Tips, Tip # 1 (San Diego Swiss) at medium frequency on the ultrasonic control base. The fine grit diamond coating on this tip allowed for smooth “sanding” of the composite around the post, and pinpoint cutting efficiency to break up the composite and flush out of the chamber.
As the reduction of composite core continued the metal post/silver point became easily visible in each access.
Once the chamber composite was cleared, and the post/silver point was found to “standing up” out of the canal, the ET25L Ultrasonic Tip (Clinical Research Dental) was then applied. This extremely long, pliable tip can be custom curved and shaped to fit into narrow space between the metal and the canal wall.
At low power, with water spray for coolant, and small radius circular motion, the metal fragments were retrieved.
The canals were then flushed, measured and instrumented to some degree of an apical stop, at file diameter size #100 for the 1.1, and diameter size #90 for the 2.1. The rough outline of the apex of 2.1, and the persistent bleed noted beyond this length suggested apical root resorption has also been occurring at this root apex.
After irrigation and drying, the canals were filled with calcium hydroxide (Ultra Cal, Clinical Research Dental), and access openings were closed with flowable composite to ensure a seal. A check appointment was tentatively scheduled in 4 weeks’ time.
Appointment 2
The patient returned four weeks later, reporting no symptoms. Clinical examination revealed the fistula over the 1.1 had resolved. Re-entry was made into each of 1.1 and 2.1. The canals were flushed, checked for length and shape, and then prepared for obturation. With the large diameter apices, the decision was made to create an apical plug of Mineral Trioxide Aggregate. The objectives were to optimize healing potential in a surgical site, and in the event that a 2nd surgery was to be contemplated, the presence of MTA already at the apex would minimize root handling and a retroseal would not be necessary after beveling.
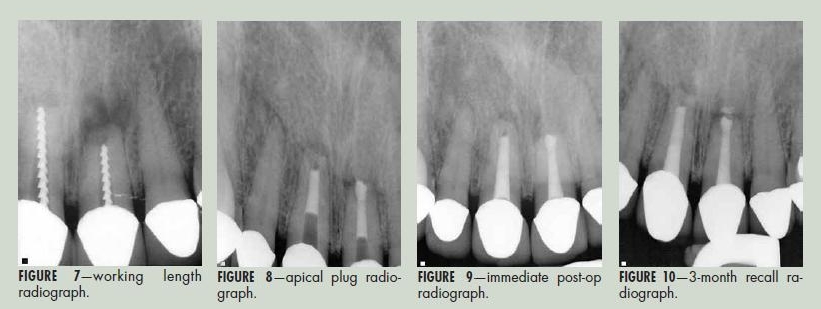
A barrier of synthetic collagen membrane (NeoCote) was placed in the canal of each tooth, and pushed to the working length with obturation pluggers. Once this soft “stop” was created, Mineral Trioxide Aggregate (MT Angelis, Clinical Research Dental) was mixed, loaded into a Dovgan carrier (Clinical Research Dental) and inserted into the canal. The MTA was inserted and condensed until a 5mm apical plug was created.
After the apical plugs were checked, the canals were back-filled with sealer and thermoplastic gutta percha in the usual fashion. Access was closed, and the patient was referred back to his family dentist for new core restorations.
RECALL APPOINTMENT
Three months after obturation, the patient returned. He reported no symptoms. The soft tissue buccal to the operative teeth remained “blue” from the metal corrosion, but displayed no fistula or discomfort on palpation or probing. A one-year recall is planned.
DISCUSSION
The key points leading to success (short term so far) in this case are that 1) the patient was the driving force in deciding to try and save his teeth in a very compromised situation, 2) the canals were able to be decontaminated by removing the obstacles, and 3) advances in dental technology and materials (optics and illumination of the microscope, ultrasonic tip designs, mineral trioxide aggregate) allowed access to and placement of materials in otherwise unreachable spaces.
The patient realizes that there may come a time when these teeth have to be replaced, but if that time frame can be pushed back another 5, 10 or even more years, then we have maintained his natural dentition that much longer – which is the primary goal of endodontics, simple or complex. OH
Dr. Steve Cohen is the on-staff Endodontist at Sunnybrook Health Sciences Centre, Department of Dentistry, is a Dental Advisor for CDPA (Canadian Dental Protective Association), and maintains a private practice limited to Endodontics in Mississauga, Ontario.
Click to download PDF: Dr. Steven Cohen, DDS - Endodontic Case Report
 Loading... Please wait...
Loading... Please wait...